Hysteresis in Lung Mechanics
Updated 12 Aug 2025 08:32
Yes, we're already title-dropping in episode two.
Why hysteresis? What even is this elusive sounding term?
The term comes from the ancient Greek ὑστερέω (husteréō), which means to 'come later' or 'lag behind'. This I believe a fitting description of physiological processes in general.
Hysteresis describes any system whose future state depends not just on current input, but also on prior states, i.e. its history.
Hysteresis can be seen in nature in various settings, but here we will limit the scope to hysteresis in the context of lung compliance, specifically the static variant.
Firstly, some definitions.
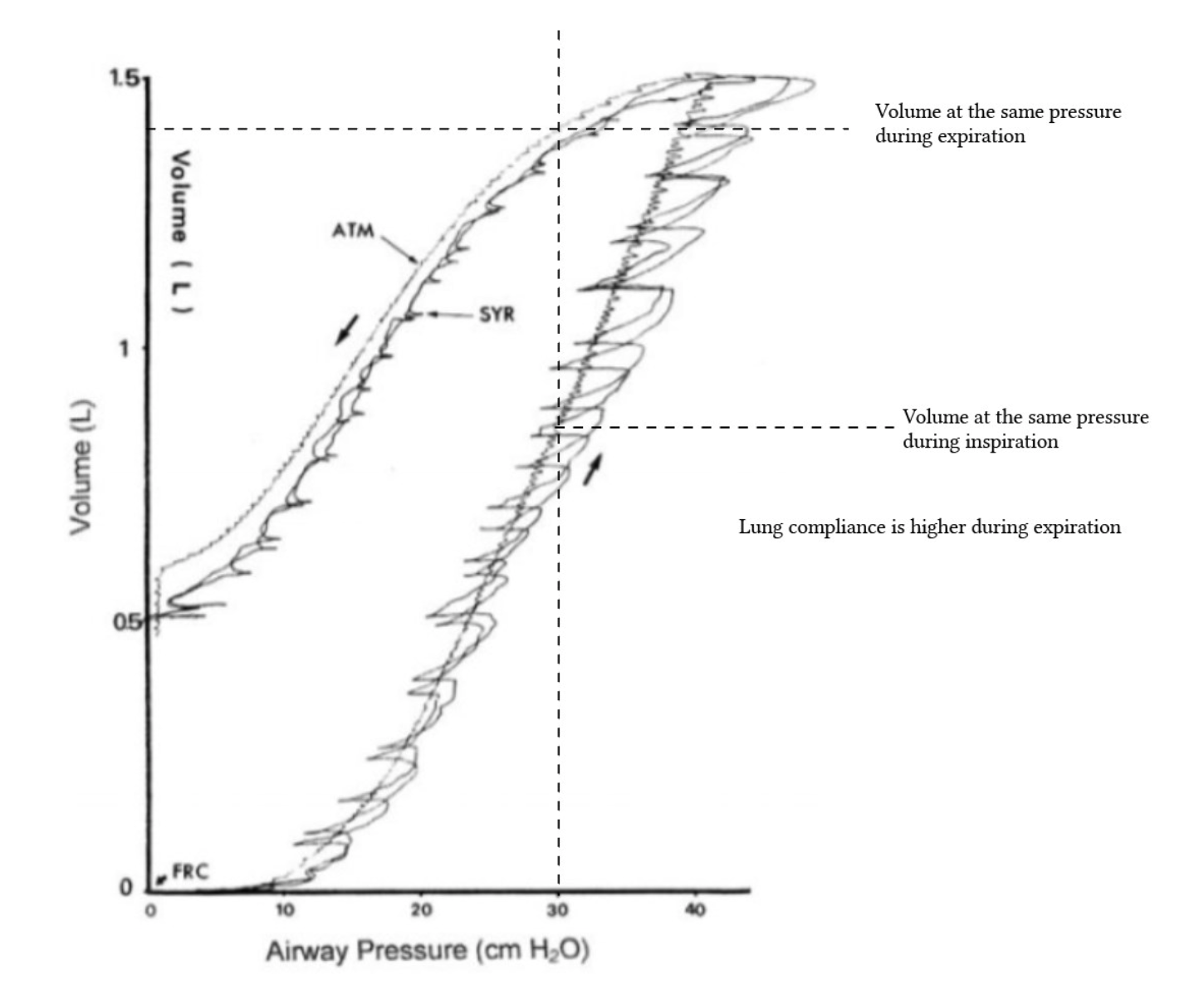
Compliance, by strict definition, is the change in volume of the lungs per unit change in pressure, and this can be defined for both inspiration and expiration.
I.e. in inspiration a positive change in pressure results in a positive change in volume, while in expiration a negative change in pressure results in a negative change in volume.
So we could break down compliance further and define inspiratory compliance and expiratory compliance separately, with inspiratory compliance having a positive ΔP and expiratory compliance having a negative ΔP.
But most of the time when people refer to 'lung compliance', they refer to inspiratory compliance, or how easily the lungs DISTEND in response to positive transpulmonary pressure (resulting in some confusion, which will be discussed later). Harris et al. (2005) describes this as 'chord compliance', noting:
For example, an increase in static compliance after a PEEP increase on a ventilator could mean simply a shift in location on the P-V curve, rather than a change in intrinsic properties of the lung.
Static lung compliance is when the volume of the lungs at a particular transpulmonary pressure is measured under STATIC conditions, i.e. when there is no gas flow, so the effects of airway resistance are removed. This in theory allows us to isolate solely the elastic properties of the lung (and if we want to be precise, the chest wall).
Transpulmonary pressure is the pressure holding the lungs open, or the pressure that pushes outwards against the natural tendency of the lungs to recoil inwards. Alveolar pressure minus pleural pressure.
Hysteresis in the context of lung compliance is the REASON that the expiratory limb of the pressure-volume curve is above the inspiratory limb, i.e. at any transpulmonary pressure, the lung volume is higher during expiration than during inspiration.
Keep in mind the DEFINITION of lung hysteresis is not the above, hysteresis is the CAUSE for the above effect.
We have not yet defined hysteresis, but will uncover this in the course of this discussion.
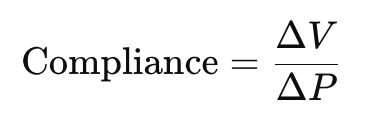
The Pressure Volume Curve
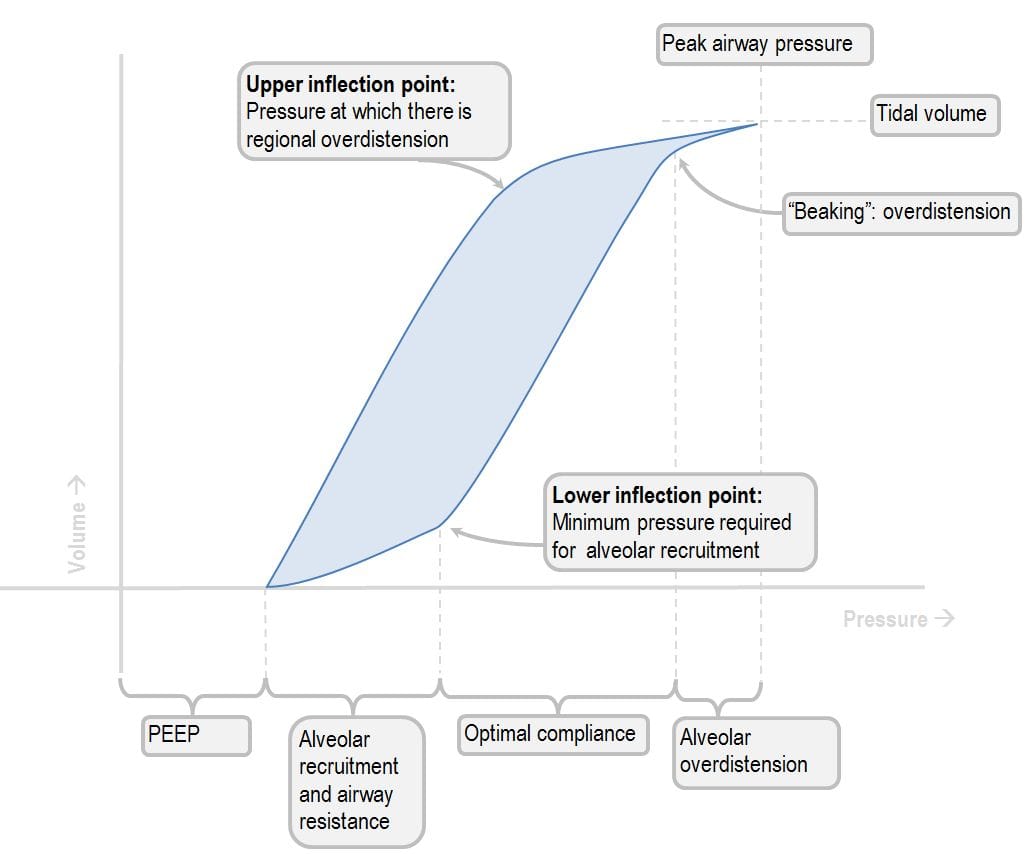
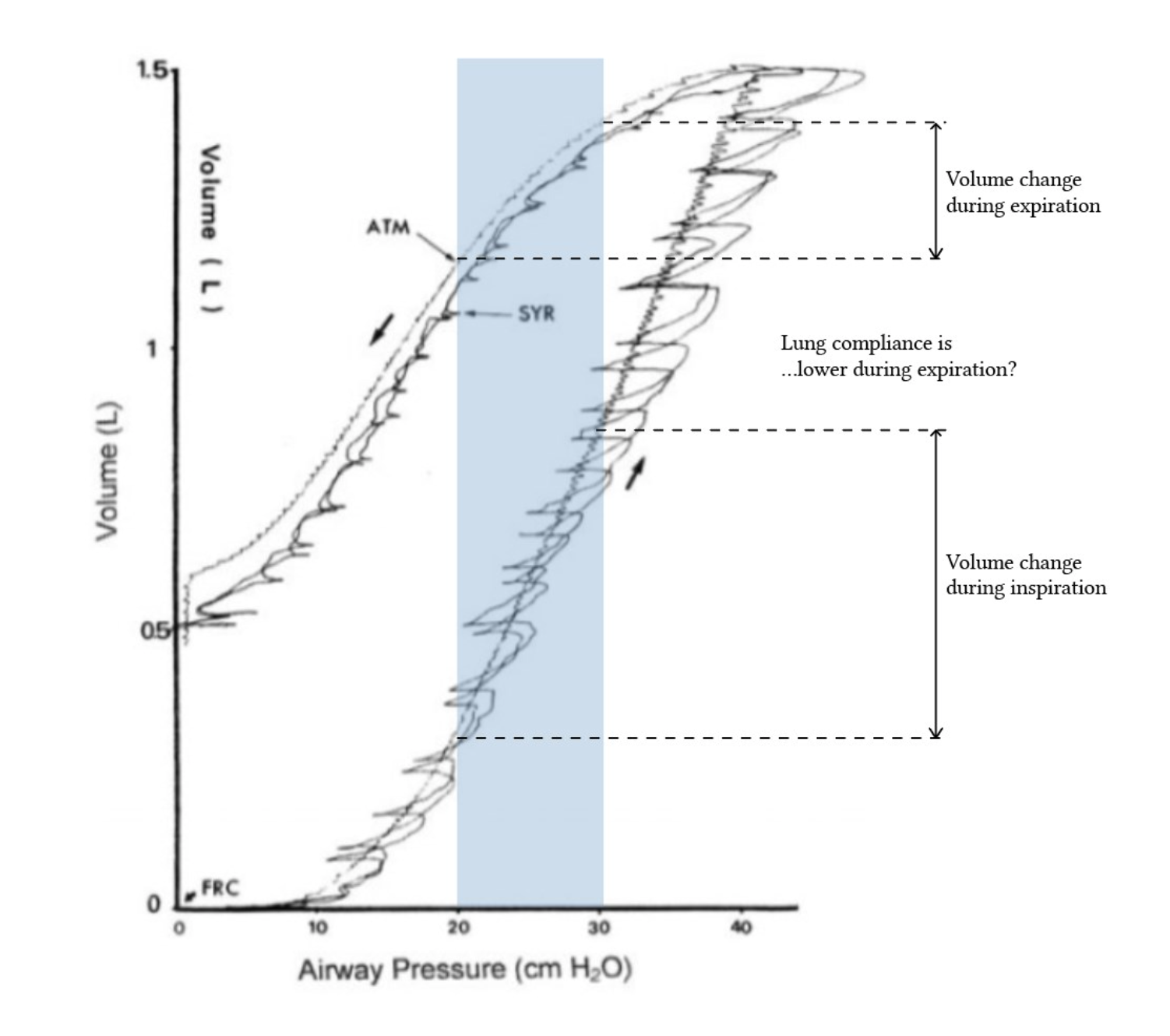
The above (brazenly plundered from Deranged Physiology) illustrates the pressure-volume curve on inspiration and expiration. Given that compliance is volume/pressure, it follows that the slope of the curve represents compliance of the lung, regardless of a positive (on inspiration), or negative (on expiration) slope, using the strict definition of compliance.
This leads most resources to describe the expiratory limb as being more compliant compared to inspiration.
But if you actually look at the slope of the expiratory limb at the start of expiration, you will find that it is actually flatter than that of the end of inspiratory limb, i.e. for the same ΔP there is a smaller ΔV. Surely this suggests that the expiratory limb is in fact LESS compliant? So are all the textbook authors describing the expiratory limb as more compliant under some sort of shared delusion, or perhaps part of a secret cult dedicated to spreading P-V curve misinformation?
Well, no. As is often the case, the reality is not quite as thrilling as conspiracy.
The frame of reference that they are operating under is simply different. They are using the more popular (but arguably less accurate?) definition of compliance, i.e. compliance being how easily the lungs EXPAND in response to positive transpulmonary pressure.
Under this frame of reference, the claim that compliance is higher on expiration is true. If we are measuring ΔP from P=0, for the same increase in pressure from P=0, there appears to be a greater increase in volume on the expiratory limb (i.e. at the SAME transpulmonary pressure the volume is higher for the expiratory values).
But is there actually any value in defining expiratory compliance this way? Well yes and no, depending on our frame of reference (everything is relative).
Firstly, my argument for why not:
Defining expiratory compliance based on a positive pressure change from zero is almost entirely meaningless in practice, as it is dissonant which what happens in reality. On the expiratory limb we are not increasing pressure from zero to achieve an increase in volume. In fact, we are going the other way, i.e. we measure relative from when the lungs are fully inflated and the ΔP would be negative, i.e. we are applying negative transpulmonary pressure (or rather we are simply passively reducing transpulmonary pressure) during exhalation. Thus defining compliance using a positive ΔP while traversing the expiratory limb is conceptually flawed. For the same negative ΔP from maximal inflation there would actually be a SMALLER decrease in volume compared to the inspiratory limb (although ironically in the same sense it would also be meaningless to discuss negative ΔP in the case of inspiration).
Now my argument for why there is value (with some reframing):
The DECREASED compliance (strict definition) at the start of the expiratory limb, (i.e. flatter slope), is actually what leads to the absolute volume magnitude on the expiratory limb to be larger than the absolute volume magnitude for the inspiratory limb at the same absolute pressure value. As pressure decreases, volume decreases too, but not as much as it 'decreases' on the inspiratory limb. This leads to higher volumes on the expiratory limb for the same absolute pressure measured from zero.
Yes, defining 'compliance' for the expiratory limb by a positive ΔP is physically meaningless. But if we reframe this as the phenomenon of the absolute volume magnitude on the expiratory limb being larger than the absolute volume magnitude for the inspiratory limb at the same absolute pressure value (which is what people mean when they talk about compliance on the expiratory limb), then this is true and has value, because this is the end result of hysteresis.
Alas, calling this increased compliance on the expiratory limb is common, but technically inaccurate shorthand.
So the statement 'compliance is higher on the expiratory limb' using the casual definition of compliance is true, but it does not match the strict definition of compliance. The meaning is useful, but the wording is misleading. The key point is that for a given pressure, the volume is greater during expiration due to hysteresis, but NOT because of a fundamentally higher compliance. Compliance is a SLOPE, not a position. Direction must be considered.
What actually is lung hysteresis?
Now that we have defined the effect of hysteresis as the absolute volume values on the expiratory limb being higher than those on the inspiratory limb for the same given pressure, we will discuss WHY that is the case, i.e. hysteresis.
Hysteresis = lag. The system's state being dependent on its history.
In terms of lung compliance, the pressure required to inspire is dependent on the lungs being initially deflated. The pressure required to expire is dependent on the lungs being already inflated. History = are the lungs inflated or deflated at the start? Result = difference in system state, i.e. different absolute volume values on the expiratory vs inspiratory limb.
The major cause is surfactant/surface tension lag, along with other causes such as alveolar recruitment/de-recruitment, stress relaxation, as well as artefact related to gas diffusion during measurement (as explained by Deranged Physiology/Harris et al. (2005)).
Surfactant/Surface tension lag
First of all what is surface tension?
Liquid molecules have cohesive forces between them, pulling them together. This inward pull creates tension at the surface of the liquid (surface tension!), which causes the liquid to minimise its surface area. It's why a small volume of water forms a spherical droplet rather than simply spreading thinly across a surface.
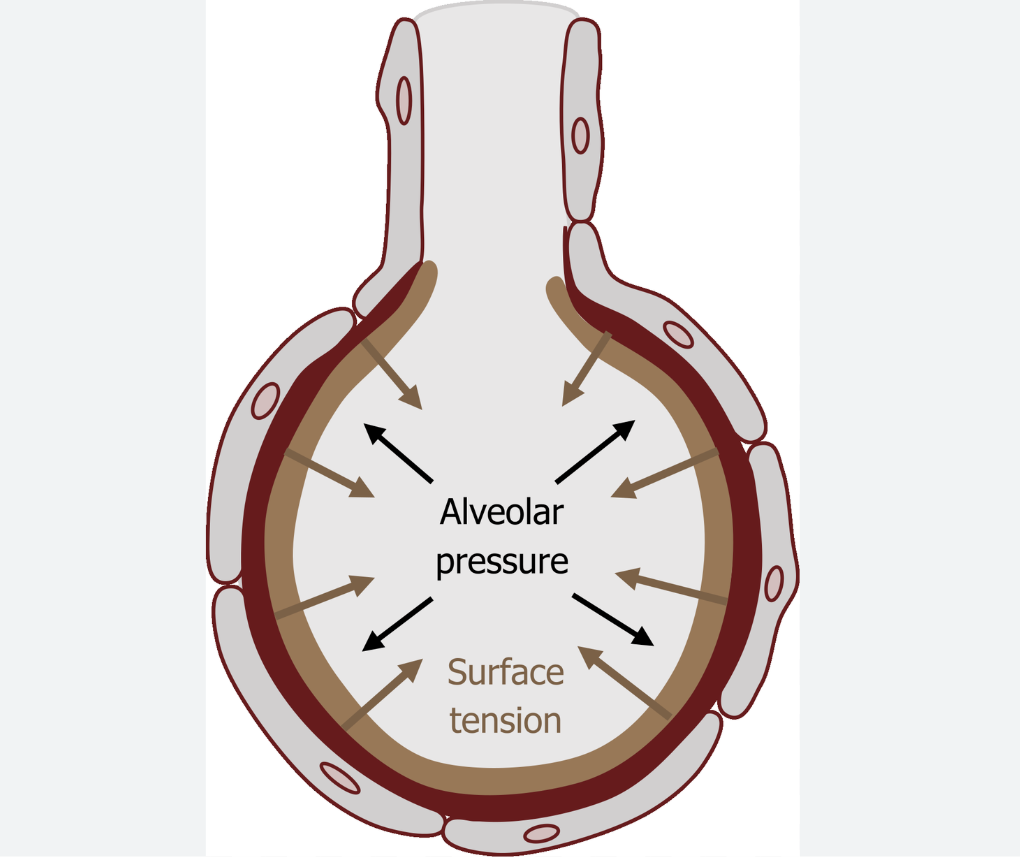
The alveoli are lined with a thin layer of fluid, and the cohesive forces between the water molecules (which are attracted to each other more strongly than to air molecules), creates surface tension, which is a force pulling the alveoli in, i.e. a collapsing force.
La Place's law
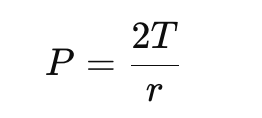
where
P = pressure needed to keep the alveolus open
T = surface tension
r = radius of the sphere (in this case the alveolus)
illustrates this - at higher levels of surface tension a greater transpulmonary pressure is required to keep the alveolus open.
Without a mechanism to counteract this, the alveoli would completely collapse.
Pulmonary surfactant, produced by type II pneumocytes, is what modulates surface tension in the lungs (by breaking up the cohesive forces between the water molecules), and prevents the alveoli from collapsing.
So back to surfactant lag.
During inspiration, at very low lung volumes, some alveoli may be completely shut, i.e. there is a water-water interface, resulting in a very high surface tension, so more pressure is required to expand the lung, until the lower inflection point of the inspiratory compliance curve is reached, which is where the alveoli snap open. At low volumes (but where the alveoli are still open), surfactant molecules are densely packed, so surface tension is reduced significantly, so the inspiratory compliance is higher. But as the lungs inflate, the alveolar surface tension increases faster than surfactant can redistribute. This 'lag' in surfactant redistribution means that surface tension rises, which reduces compliance as inflation continues. So inspiratory compliance progressively falls as alveoli stretch and surfactant becomes less concentrated on the surface.
During expiration, the surfactant has already been spread thin due to prior inflation, but it has had the time spread evenly, i.e. is already in place, so it prevents rapid volume loss. As the alveolar surface area decreases, surfactant molecules re-concentrate rapidly, reducing surface tension. Importantly, this re-concentration is more immediate than its spreading was during inspiration. It does not lag as much. Surface tension stays low, and alveoli resist collapse. Thus a given fall in pressure leads to a smaller fall in volume. This makes the expiratory P-V curve sit above the inspiratory one.
Tldr: during inspiration, surfactant molecules lag behind alveolar expansion, causing surface tension to rise, and reducing compliance. In contrast, during expiration surfactant is already distributed and quickly re-concentrates as the alveoli shrink, maintaining low surface tension and preventing alveolar collapse. This leads to higher absolute lung volumes at any given pressure on the expiratory limb, not because the expiratory limb is more compliant, but because of reduced surface tension and surfactant 'readiness' during deflation.
But there is a seeming local inconsistency. At small lung volumes, surfactant is more concentrated so surface tension is low, while at high lung volumes surfactant is more spread thin, so surface tension will be higher. But doesn't that mean when the lungs are fully expanded, surface tension will be high at the start of expiration, so there would be a greater drop in volume per drop in volume as the patient expires? But the actual observed slope of at the start of the expiratory limb is more flat.
Well, we need to remember that static P-V curves are not dynamic recordings. We are looking at the quasi-static pressure-volume relationship, i.e. we are measuring lung volume after there is some equilibration. So even if surfactant is initially less effective at high lung volumes, by the time you are taking that data point on the expiratory curve, surface tension has already normalised as surfactant has had time to re-concentrate during deflation. Surfactant during expiration re-concentrates quickly. As the lung deflates alveolar surface area decreases faster than surfactant is cleared/degraded, so surfactant molecules repack tightly together, leading to rapidly surface tension. This effect is immediate and dominant in early expiration which stabilises alveoli and limits volume loss per pressure drop.
But then you may ask, if we are measuring quasi-static values, wouldn't surfactant also have time to equilibrate during the inspiratory limb? Well, kind of, but there is not enough time. Surfactant can rapidly re-concentrate during deflation. As alveoli shrink, surface area drops. The same amount of surfactant molecules are now spread over a smaller surface, so the concentration of surfactant increases automatically. No active process is required. The passive re-concentration results in rapid surface tension reduction. But during inflation, surfactant must actively spread. As the alveoli expand, surface area is increased, and the surfactant needs to redistribute across this growing surface. This is not instantaneous, so even during quasi-static conditions there is some lag in redistribution, so surface tension stays temporarily high.
Tldr: surfactant LAGS behind inflation, but keeps up easily during deflation.
Recruitment of Alveoli
As mentioned on previously, initially at the start of the inspiratory limb, there are some fully collapsed alveoli, where the inner walls are touching each other, i.e. a water-water interface which has very high surface tension, so a lot pressure is required to overcome this surface tension to open up the alveoli. Thus in the process of recruitment, lung inspiratory compliance is low.
In contrast, on the expiratory limb the alveoli are already open and the surfactant has had time to spread across their inner surfaces, so there is less surface tension compared to during recruitment. This means expiratory compliance (pressure-volume gradient) is low, but volume for the same pressure on the expiratory limb is higher than that for the inspiratory limb.
Stress Relaxation
When an elastic band is stretched and held at a constant length/strain, the force required to maintain that fixed stretched length will reduce gradually over time.
This is stress relaxation, where the stress in a material gradually decreases when it is held at a constant strain.
The same process happens in the lungs. Here, transpulmonary pressure is the stress applied, and the lung volume is the strain/stretch.
When the lungs are distended with a constant positive transpulmonary pressure, eventually some of the energy will dissipate, so the input of energy does not equate to the output. The transpulmonary pressure applied is not perfectly conserved and stored as elastic recoil. So the force of elastic recoil is smaller at the start of expiration than the gradient of the end of the inspiratory limb.
Gas diffusion during measurement of static values
When we measure static lung compliance, at each data point measured, the subject momentarily stops inspiring/expiring, creating (quasi)static conditions. But during each of these pauses, some of the gas will diffuse, which may slightly confound the measured volume changes per different pressures to some extent.
TLDR
To sum hysteresis up in extremely simple terms:
- the inspiratory limb initially rises slower - it takes more pressure to inflate the lung to a given volume.
- the expiratory limb initially falls slower - for the same pressure the lung holds more volume during deflation.
So at any given pressure the lung is bigger during deflation than it was during inflation. This mismatch is the result of hysteresis.
References
Yartsev A. Static, dynamic and specific compliance. Deranged Physiology: CICM Primary Exam – Respiratory System.
Yartsev A. Interpreting the shape of the pressure–volume loop. Deranged Physiology: CICM Primary Exam – Respiratory System.
Harris, R. Scott. "Pressure-volume curves of the respiratory system." Respiratory care. 2005; 50(1):78-99.
Wijayasiri L, Mccombe K. The Primary FRCA Structured Oral Exam Guide 1. 2nd ed. London: CRC Press; 2017.
Nickson C. Compliance. Part One – LITFL.
Binks A. Pulmonary Physiology for Pre-Clinical Students; 2022.